7 Natural Supplements For Optimizing Fertility In Men And Women
DISCLAIMER:This blog does not intend to provide diagnosis...
- In this article:
- Is Infertility Common?
- What Are Common Contributors Of Male Fertility Challenges?
- What Are Common Contributors Of Female Fertility Challenges?
- What Lifestyle Changes Can Help Improve Fertility Success?
- What Supplements Could Help Increase Fertility?

Is Infertility Common?
Infertility is a common problem faced by up to 15 percent of the population worldwide. Usually defined as difficulty conceiving after one year of having intercourse at least twice per week, without the use of birth control, infertility is estimated to affect up to 50 million couples globally.
The inability to conceive can create depression and anxiety amongst those desiring children. In couples, infertility can be attributed to the male partner 30 to 40 percent of the time, while the woman may account for 60 to 70 percent of the challenges resulting in a nonviable pregnancy.
Despite this, male infertility may be increasing. A 1992 study in BMJ found that between 1938 and 1991, male semen volume and sperm count significantly diminished. Another study found that between 1980 to 2015, sperm counts dropped 57 percent throughout North America, Asia, Europe, and Africa. A popular theory identifies industrialization as the cause.
No matter the source, fertility issues are often complex and will generally require both partners’ cooperation and focus to overcome. We will discuss what natural approaches may help improve the odds of becoming pregnant and bringing a healthy child into the world.
What Are Common Contributors Of Male Fertility Challenges?
- Low sperm count (commonly caused by stress, tobacco use, obesity, marijuana, and excess alcohol)
- Low quality of sperm (commonly caused by stress, tobacco use, poor nutrition, environmental toxins, obesity, marijuana, and excess alcohol)
- Varicocele (a varicose vein in the scrotum that can usually be fixed by a urologist)
- Chronic infections (untreated or delay in treatment of sexually transmitted infections)
- Ejaculation issues (i.e. retrograde)
- Impotence (commonly caused by psychological sources, history of radiation and chemotherapy, surgery, and low testosterone)
- Genetic variations (Klinefelter's syndrome or Kallman syndrome)
What Are Common Contributors Of Female Fertility Challenges?
- Polycystic ovarian syndrome (common in more than 10% of women)
- Advanced maternal age (i.e. over age 35)
- Insulin resistance (high-carbohydrate diet, high-sugar diet)
- Endometriosis
- Premature ovarian failure (hormonal issues)
- Damage to fallopian tubes (due to past infections of gonorrhea or chlamydia)
- Uterine or cervical issues (abnormal uterine shape, cervical stenosis, etc.)
- Recent use of contraceptive medications (may take over one year for the body to reset)
What Lifestyle Changes Can Help Improve Fertility Success?
Making healthy choices is not only good for the heart and brain but also can help improve the likelihood of becoming pregnant and having a healthy child. A well-balanced diet that is low in sugar and processed foods is paramount for both parents to help ensure a healthy internal environment is present to create a human life. Consuming a Mediterranean diet, for instance, maybe helpful for fertility, according to some studies.
Regular exercise and quality sleep is important for healthy sperm in men and for predictable, stress-free ovulation in women. Avoiding environmental toxins such as BPA (bisphenol-A) and other chemicals in plastics is also advisable as they can act as hormone disruptors. Limiting exposure to heavy metals such as lead and mercury should also be considered. Hand soaps that contain triclosan should be avoided. In 2017, the United States banned this soap additive due to studies linking it to poorer semen quality.
Some studies have also suggested that electromagnetic radiation, like that from WiFi (Wireless Fidelity), may also contribute to reduced sperm quality. More studies are, however, needed to confirm this.
Avoiding drugs, tobacco, and excessive alcohol is not only important when trying to conceive but also important to help ensure a healthy pregnancy.
Achieving an optimal weight when trying to become pregnant is also important. Having insulin resistance or prediabetes is a well-known risk factor that can make conception difficult for many women. Women with diabetes are also at an increased risk for developing complications during pregnancy and delivery and are considered at higher risk.
What Supplements Could Help Increase Fertility?
In addition to the lifestyle changes, the following 7 supplements may also be helpful according to studies.
Berberine
Berberine is extracted from the barberry (berberis vulgaris) shrub, which contains both evergreen and deciduous plants and is found throughout Europe, North Africa, the Middle East, and Asia. Berberine, its active ingredient, is consumed as an herbal food and supplement. It has been shown in scientific studies to have various health benefits and is commonly used in Traditional Chinese Medicine (TCM) and ayurvedic medicine.
Polycystic ovarian syndrome (PCOS) is a common cause of infertility and is present in up to 10 percent of all women. Diagnosed by a simple blood test, PCOS disrupts hormones, and insulin resistance and prediabetes are also usually present in this condition. Diet and exercise are crucial for the reversal of PCOS, and berberine also appears to be a useful supplement.
A 2012 study showed that berberine could be helpful in reducing insulin sensitivity (a symptom of PCOS), which ultimately helps to lower glucose levels while restoring a more normal menstrual cycle. A previous 2010 study in Biochemical Pharmacology showed that berberine activated GLP-1, which promotes insulin secretion and ultimately helps control blood glucose and insulin resistance, another benefit for those with PCOS.
Suggested dose: As directed on the label.
L-Carnitine
L-carnitine is an important amino acid found in high concentration in both muscles and the brain. It also plays an important role in the production of energy and metabolism and may play a role in fertility.
A 2015 randomized, double-blind, placebo-controlled study of 60 women with PCOS (Polycystic Ovarian Syndrome) included participants considered overweight (BMI >25). Half the women were given 250 mg of L-carnitine, while the other 30 women were given a placebo pill. Both groups were followed for 12 weeks, and at the end of the period, those who took the L-carnitine saw a reduction in weight and waist circumference and had lower blood sugar. These changes would likely result in more predictable ovulation and subsequently improved odds for conception.
A 2014 study in the European Journal of Obstetrics and Gynecology and Reproductive Biology demonstrated that women with PCOS who were resistant to clomiphene (meaning this prescription drug could not help them become pregnant) were more likely to become pregnant when 3,000 mg of L-carnitine was added to their daily drug regimen. This is an excellent example of using both nutritional supplements and prescription drugs to achieve the desired health goal.
Suggested dose: 250 mg to 3,000 mg per day
Maca Root
Maca root (lepidium meyenii) is an adaptogenic herb cultivated in the Andes Mountains of South America and grows at elevations of 13,000 to 16,000 feet (4000-5000 m) above sea level. Traditionally used by the Incas, maca was known for its numerous medicinal benefits and primarily used to improve both libido and fertility. It was and still is considered an aphrodisiac by many.
Studies of men have shown that maca root can enhance sperm count and the motility of sperm. A 2002 double-blind, placebo-controlled study demonstrated that men who took maca root had improved sexual desire when compared to those who took a placebo pill. A 2009 study in Andrologia showed improvements in sexual function in men with mild erectile dysfunction.
Suggested dose: As directed on the label
Pine Bark
A potent antioxidant, pine bark extract was originally used by indigenous people of North America and Asia as a medicinal herb. French expeditioner Jacques Cartier reportedly used pine bark extract in 1535 during his expedition as a treatment for scurvy, a condition caused by insufficient levels of vitamin C intake.
Today, integrative healthcare professionals have also realized the many health and anti-aging benefits of pine bark extract, which was first introduced into the United States as a dietary supplement in 1987.
Pine bark extract (pinus masonianna from Asia) is one of the most common formulations used, while French maritime pine bark extract or Pycnogenol® (pinus pinaster ssp. Atlantica is from Europe) is a patented blend of this powerful nutrient.
A 2015 study from Italy showed Pycnogenol and L-arginine could improve the quality of sperm. In addition, a 2002 study also showed improved sperm quality when pine bark was supplemented.
Suggested dose: As directed on the label.
Prenatal Vitamins
Women who are trying to conceive should take a prenatal vitamin. While it is common for women to start taking a vitamin once they become pregnant, this is not ideal as many women usually learn they are pregnant two to six weeks after conception. Ensuring that all the required vitamins and minerals are being consumed, including iodine and folate, is key to any quality prenatal vitamin and healthy pregnancy.
Potential fathers should also consider a quality men’s multivitamin to help ensure optimized sperm health and quality.
Suggested dose: As directed on the label.
Vitamin C
Vitamin C, also known as ascorbic acid or ascorbate, has been one of the most researched vitamins over the last 50 years. A search of the scientific literature reveals that over 53,000 studies have been conducted on vitamin C since 1968, including studies on the role it plays in fertility.
A 2006 study showed that “…vitamin C supplementation in infertile men might improve sperm count, sperm motility, and sperm morphology and might have a place as an additional supplement to improve the semen quality towards conception.”*** The dose given in the study was 1000 mg twice per day.
Smoking also lowers vitamin C levels in the blood. A 2006 study showed that non-fertile smokers had lower levels of vitamin C in their semen when compared to fertile men who were non-smokers. So, if you smoke, now is the time to stop!
Further, a 2016 study also showed that vitamin C supplementation was beneficial on sperm quality and quantity. Similarly, a 2020 study found that daily vitamin C helped improve sperm quality and DNA integrity when supplemented.
Suggested dose: 500 to 1,000 mg once or twice per day.
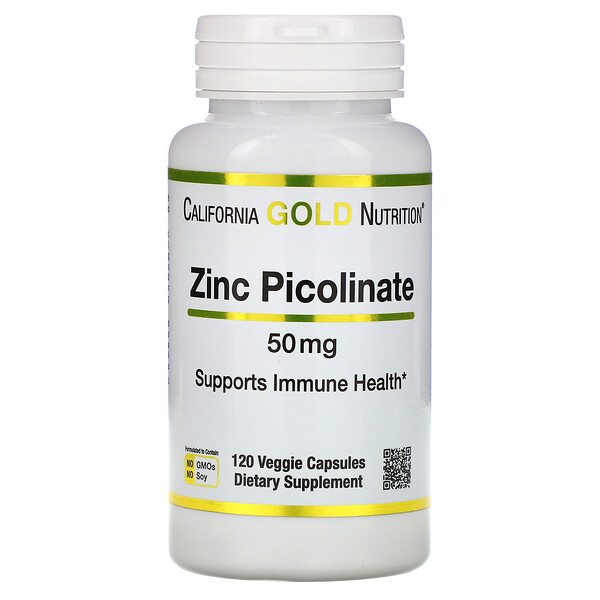
Zinc
According to the Journal of Nutrition almost 45 percent of Americans have inadequate intake of zinc in their diets. Worldwide, more than 15 percent of people are zinc deficient. The problem is very common in Sub-Saharan Africa and South Asia. Required by enzymes in the reproductive system and throughout the body, zinc is involved in over 300 biochemical reactions and is an important component of over 2,000 proteins.
A 2009 study showed that men who were most fertile had higher blood levels of zinc compared to men who were infertile. These results led researchers to conclude that, “poor zinc nutrition may be an important risk factor for low quality of sperm and male infertility.”
Zinc is required for fertilization to occur. The 2020 article “The Role of Zinc in Male Fertility” explains that zinc is required for sperm to be able to swim to their target and also for the fertilization reaction to occur. Men with low zinc levels will have sperm that is lower quality, negatively affecting their chances of biologically producing a child.
Medications that deplete zinc include acid reducers (ranitidine, famotidine, omeprazole, etc.) and ACE inhibitor blood pressure medications such as lisinopril, benazepril, and enalapril. Always consult with your physician prior to stopping any prescribed medication.
Most people can get sufficient zinc by taking a multivitamin that contains zinc. A diet rich in legumes, nuts (pine nuts, cashews, almonds), seeds (hemp, pumpkin, sesame, sunflower, and chia), eggs, and dark chocolate can also provide dietary zinc.
Other Supplements That May Help
Other supplements which have been shown to be helpful in improving sperm count and health include NAC, selenium, and coenzyme Q10.
References:
- Carlsen E, Giwercman A, Keiding N, Skakkebaek NE. Evidence for decreasing quality of semen during past 50 years. BMJ. 1992 Sep 12;305(6854):609-13.
- Sengupta P, Dutta S, Krajewska-Kulak E. The Disappearing Sperms: Analysis of Reports Published Between 1980 and 2015. Am J Mens Health. 2017 Jul;11(4):1279-1304.
- Association Between Use of Marijuana and Male Reproductive Hormones and Semen Quality:A Study Among 1,215 Healthy Young Men. Am J Epidemiol. 2015 Sep 15;182(6):473-81. 4
- Accessed March 1 st , 2021 https://www.vierafertility.com/blog/mediterranean-diet-linked-to-ivf-success/
- Liu MM, Liu L, Chen L, et al. Sleep Deprivation and Late Bedtime Impair Sperm Health Through Increasing Antisperm Antibody Production: A Prospective Study of 981 Healthy Men. Med Sci Monit. 2017;23:1842-1848. Published 2017 Apr 16.
- Jurewicz, J., Radwan, M., Wielgomas, B. et al. Environmental levels of triclosan and male fertility. Environ Sci Pollut Res 25, 5484–5490 (2018). https://doi.org/10.1007/s11356-017-0866-5
- Accessed March 1 st , 2020 https://www.bionews.org.uk/page_142704
- Li MF, Zhou XM, Li XL. The Effect of Berberine on Polycystic Ovary Syndrome Patients with Insulin Resistance (PCOS-IR): A Meta-Analysis and Systematic Review. Evid Based Complement Alternat Med. 2018 Nov 14;2018:2532935.
- Berberine improves insulin sensitivity by inhibiting fat store and adjusting adipokines profile in human preadipocytes and metabolic syndrome patients. Yang J, Yin J, Gao H, Xu L, Wang Y, Xu L, Li M Evid Based Complement Alternat Med. 2012; 2012():363845
- Modulation of glucagon-like peptide-1 release by berberine: in vivo and in vitro studies. Yu Y, Liu L, Wang X, Liu X, Liu X, Xie L, Wang G Biochem Pharmacol. 2010 Apr 1;79(7):1000-6.
- Samimi, M. , Jamilian, M. , Ebrahimi, F. A., Rahimi, M. , Tajbakhsh, B. and Asemi, Z. (2016), Oral carnitine supplementation reduces body weight and insulin resistance in women with polycystic ovary syndrome: a randomized, double‐blind, placebo‐controlled trial. Clin Endocrinol, 84: 851-857.
- Alaa M. Ismail, Ali Hassan Hamed, Srdjan Saso, Hossam H. Thabet, Adding l-carnitine to clomiphene resistant PCOS women improves the quality of ovulation and the pregnancy rate. A randomized clinical trial, European Journal of Obstetrics & Gynecology and Reproductive Biology, Volume 180, 2014, Pages 148-152
- 19. Gonzales G. F., Cordova A., Gonzales C., Chung A., Vega K., Villena A. Lepidium meyenii (Maca) improved semen parameters in adult men. Asian Journal of Andrology. 2001;3(4):301–303.
- Gonzales G. F., Córdova A., Vega K., et al. Effect of Lepidium meyenii (MACA) on sexual desire and its absent relationship with serum testosterone levels in adult healthy men. Andrologia. 2002;34(6):367–372.
- Zenico T., Cicero A. F. G., Valmorri L., Mercuriali M., Bercovich E. Subjective effects of Lepidium meyenii (Maca) extract on well-being and sexual performances in patients with mild erectile dysfunction: a randomized, double-blind clinical trial. Andrologia. 2009;41(2):95–99.
- Arch Ital Urol Androl. 2015 Sep 30;87(3):190-3. doi: 10.4081/aiua.2015.3.190.
- Roseff SJ. Improvement in sperm quality and function with French maritime pine tree bark extract. J Reprod Med. 2002 Oct;47(10):821-4. PMID: 12418064.
- Akmal M, Qadri JQ, Al-Waili NS, Thangal S, Haq A, Saloom KY. Improvement in human semen quality after oral supplementation of vitamin C. J Med Food. 2006 Fall;9(3):440-2.
- Mostafa T, Tawadrous G, Roaia MM, Amer MK, Kader RA, Aziz A. Effect of smoking on seminal plasma ascorbic acid in infertile and fertile males. Andrologia. 2006 Dec;38(6):221-4.
- Ahmadi S, Bashiri R, Ghadiri-Anari A, Nadjarzadeh A. Antioxidant supplements and semen parameters: An evidence based review. Int J Reprod Biomed. 2016;14(12):729-736.
- Hamidian S, Talebi AR, Fesahat F, Bayat M, Mirjalili AM, Ashrafzadeh HR, Rajabi M, Montazeri F, Babaei S. The effect of vitamin C on the gene expression profile of sperm protamines in the male partners of couples with recurrent pregnancy loss: A randomized clinical trial. Clin Exp Reprod Med. 2020 Mar;47(1):68-76.
- Ciubotariu D, Ghiciuc CM, Lupușoru CE. Zinc involvement in opioid addiction and analgesia – should zinc supplementation be recommended for opioid-treated persons? Substance Abuse Treatment, Prevention, and Policy. 2015;10:29.
- Wessells KR, Brown KH. Estimating the Global Prevalence of Zinc Deficiency: Results Based on Zinc Availability in National Food Supplies and the Prevalence of Stunting. Bhutta ZA, ed. PLoS ONE. 2012;7(11):e50568.
- Andreini, C.; Banci, L.; Bertini, I.; Rosato, A. Counting the zinc-proteins encoded in the human genome. J. Proteome Res. 2006, 5, 196–201. [
- Colagar AH, Marzony ET, Chaichi MJ. Zinc levels in seminal plasma are associated with sperm quality in fertile and infertile men. Nutr Res. 2009 Feb;29(2):82-8
- Allouche-Fitoussi D, Breitbart H. The Role of Zinc in Male Fertility. Int J Mol Sci. 2020;21(20):7796. Published 2020 Oct 21.
- Safarinejad MR, Safarinejad S. Efficacy of selenium and/or N-acetyl-cysteine for improving semen parameters in infertile men: a double-blind, placebo controlled, randomized study. J Urol. 2009 Feb;181(2):741-51.

 By Dr. Eric Madrid, M.D.
By Dr. Eric Madrid, M.D.